We are thrilled to announce that Southwest Medical Specialists (SWMS) has joined Brellah, marking a significant milestone in our journey to provide exceptional healthcare to our community.


We are thrilled to announce that Southwest Medical Specialists (SWMS) has joined Brellah, marking a significant milestone in our journey to provide exceptional healthcare to our community.
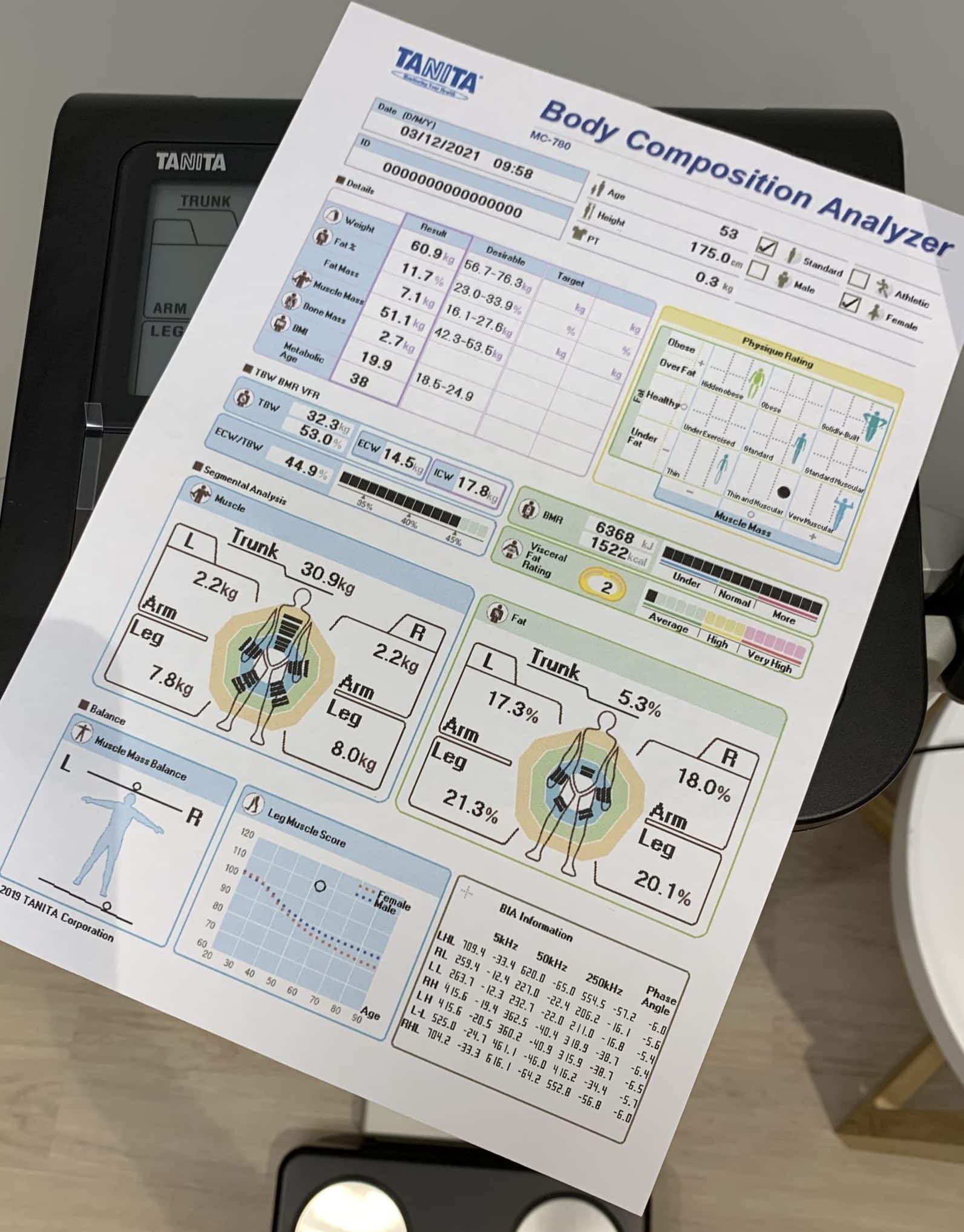
Body composition scanning is a useful, non-invasive way to measure how much fat, muscle and bone mass you have.

Did you know two in three Australian adults are considered to be overweight or obese?

We believe in actively challenging the healthcare paradigm to impact better health outcomes for all involved.